Bag Valve Mask Study, Part I
What’s a bag valve mask and what’s wrong with it?
In emergency medical services, the need for bag valve mask (BVM) ventilation is a common occurrence. BVMs are used at all levels of care, from CPR certified civilians to anesthesiologists, for a wide range of call types. BLS and ALS practitioners are trained to use BVMs for cardiac arrests, altered levels of consciousness, asphyxiation, and other calls that can result in or from the patient became apneic. Although it has proved to be a vital piece of equipment, there is an unmet medical need in this area for a way to improve the ease of achieving an airtight seal between the mask and face of patients in respiratory distress to deliver maximum oxygen at consistent tidal volumes.
A careful review of the unmet need for ventilation masks narrowed the primary stakeholders involved at all levels of pre-hospital care into three main categories: 1) patients, 2) administrators, and 3) medical providers.
As the group directly receiving care, patients experience the effectiveness of ventilation. If the provider on hand is unable to correctly position both the mask and the patient’s head, oxygen is lost and can negatively impact the patient’s health and prognosis. Therefore, as a stakeholder, patients care about how effective their treatment is administered.
A second stakeholder is the administrators. More specifically, the purchasing department - which can be made up of supervisors, medical directors, or purchasing specialists - need to provide masks to all ambulances as well as ensuring that the ventilation masks work effectively and reliably. Because of the frequent need for these masks in various scenarios, a key concern for administrators is to maximize effectiveness while simultaneously minimizing cost. Many ventilation masks are designed to be reusable with replacement filters that can withstand a disinfection regimen in between uses, so equipping ambulances and providers with high-quality masks can be cost-effective in the long term due to a less frequent need for replacement. Current designs are often equipped with a plastic air-cushion which directly interfaces with the patient’s face. With use and time, the plastic air-cushion often deflates, deforms, or cracks making forming an air-tight seal quite difficult. Another consideration with cost is wasting material. If the seal between mask and face is not airtight, that means oxygen is leaking out the sides. Not only is the patient not getting all the oxygen, but this would deplete the oxygen tank a lot faster, wasting essential supplies.
The final, and principal, stakeholders involved, are the pre-hospital medical providers on the scene directly using and interacting with BVM ventilation. These providers (BLS and ALS) receive training on how to properly ventilate patients. This entails learning the proper techniques for achieving an air-tight seal during ventilation, holding the patient’s head in the right posture to open the airway, and delivering the right tidal volume. In practice, it is essential for the provider to pay extra attention during each step and throughout the care process due to the wide variability in facial shapes and features. Key indicators of correct BVM use is observing expected levels of chest rise and feeling for any air leaks surrounding the mask. Unfortunately, this task can be tricky on the scene, especially when there is only one provider using the BVM. According to a survey conducted for this project in February 2019, a majority of responders at all levels indicated being the sole provider using the BVM at least 50% of the time they were using the device. Said survey also indicated that creating and maintaining a seal was the most frequent complication these providers faced. Thus, a mechanism to improve the interface between mask and face has the potential to reduce air leaks, minimize hand fatigue, and allow rapid removal and replacement of masks for unpredictable events (e.g., vomit) can severely improve ease of use and improve the effectiveness of care.
What should be done?
To improve the ease of use for the providers, our solution proposes replacing the pneumatic face cushioning of the original BVMs with a formable gel. The new gel cushioning will help the users create a better seal against a wider variety of face sizes and shapes and minimize the amount of force the users must exert on the patient’s face to establish this seal. Additionally, our modifications will include an assistive ledge at the bottom of the mask to help the user maintain the necessary “head-tilt, chin-lift” motion required to open the patient’s airway. This added component will improve oxygen delivery by allowing the users to focus on creating the seal without having to worry about simultaneously gripping the patient’s chin to establish this open airway, thus reducing the likelihood of broken seals and improving oxygen delivery.
To satisfy our goals, this improved BVM must be biocompatible when placed against the patient’s skin. Because of the external nature of this device, this mask must be completely bioinert, even in cases where facial tissue may be lacerated, burned, or otherwise damaged. The mask must also not contain any allergens, irritants, or toxins to ensure that it will perform with minimal host response.
The materials used for this mask must meet the requirements set of flexibility, durability, and opacity. The mask must be flexible enough to fit on all patient facial structures while remaining sturdy enough to function effectively for the entire duration of its use. The mask should be made with materials that can retain elasticity and maintain chemical integrity through many cycles of use during the life of the product. Lastly, the material of the mask must be transparent to enable the user to see through the mask to view airflow and patient status. Alternatively, this last point can also be satisfied through other ways of allowing EMS personnel to understand patient status.
To ensure product adoption, it is imperative that the mask can be integrated into older BVM systems. The mask must be compatible with attachments and accessories for different uses. This modularity may allow for a cohesive ecosystem in which this the product may be used for multiple purposes. Quick mask deployment and removal must be able to still be accomplished using this new mask. The product must be easily affixed to the patient’s face as well as quickly removable in event of complications such as patient vomiting. Mask adoption also relies on the new product being easier to use than the incumbent design. The mask must be easily held by a variety of hand sizes in addition to a range of face sizes. The user should be able to effortlessly maintain a tight grip. The mask’s inherent ease of use will facilitate operation by newly trained or untrained personnel.
Finally, the product must fit a variety of patient facial features. The product must be able to maintain a tight seal on a range of different types of facial structures and in the presence of facial hair.
Design Documentation
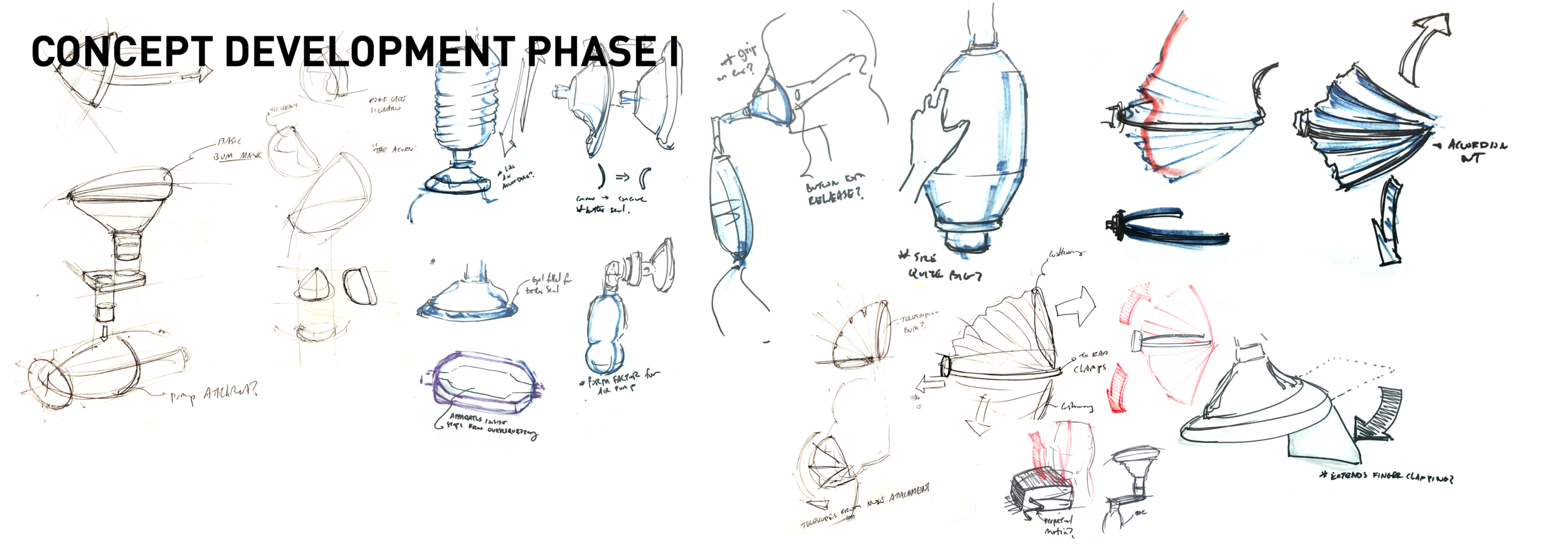
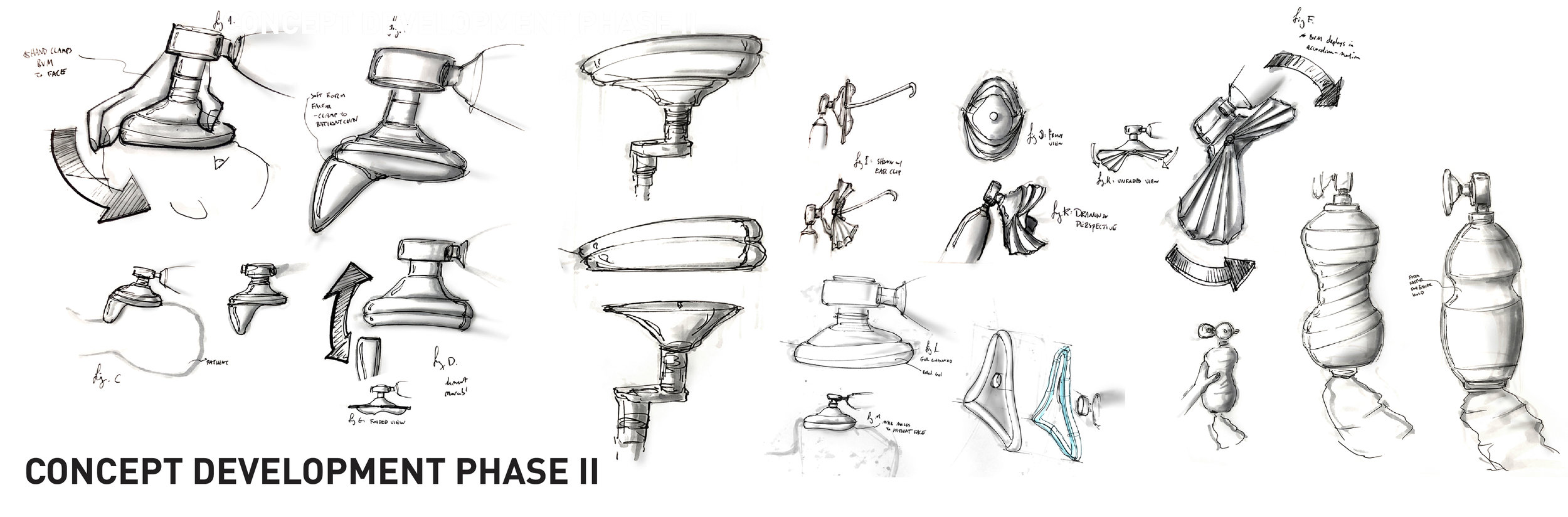
Our first round of ideation focused various ways to create a better seal, including the gel concept we have discussed so far. We also considered a strap to hold the cushion in place, which would be combined with a removable plastic shell to make the oral and nasal cavities immediately accessible if needed. Our first rounds of concept development also focused on changing aspects of the bag itself, but after conducting the survey, we decided to divert our attention to the mask. Also, after receiving some feedback from our colleagues at the end of last class, we decided to put a hold on the strap and removable frame concept for the time being to focus exclusively on the cushion and chin attachment.
What are we going to prototype?
Our prototype focuses on selecting and testing the gel cushion and on the development of the chin attachment. At this point, we are still in the process of materials selection to determine the ideal medical grade thermoplastic elastomer. However, for our initial “works-like” model, we are using a borax-based slime mixture to create a gel-like material for initial concept testing. Our first priority is to test our claim that a filled cushion is better than the current pneumatic model. Once we decide on the material for the supplemental gel, the concerns about shelf life and sterilization will be easier to address. Simultaneously, we are focusing on creating the assisted “head-tilt, chin-lift” attachment. We are currently working on developing a specific shape of the attachment that maximizes comfort on the sensitive throat area. By the end of the semester, we are planning on testing our new mask on airway and CPR mannequins.
Medical Device Realization, Spring 2019
Group 2: Team Lifesavers
Chanel Jhin, Molly Kaissar, Matthew Smeltzer, Brian Xiao